*MEDICATION-ASSISTED TREATMENT OF OPIOID DEPENDENCE/OPIOID USE DISORDER


The First Stage: Intake
At this preliminary stage you will be given a comprehensive substance use disorder/dependence assessment, as well as an evaluation of mental status and physical exam. The pros and cons of the treatment medication chosen will be presented. For opioid agonist treatment (OAT), opioid (“agonist”) medications are used. It will be either Methadone or a Buprenorphine product. These have an opiate effect similar to that of the opioids to which you have become psychologically dependent. Treatment expectations, compliance, as well as commonly occurring issues involved with maintenance treatment and medically supervised withdrawal (“detox”), will be discussed.
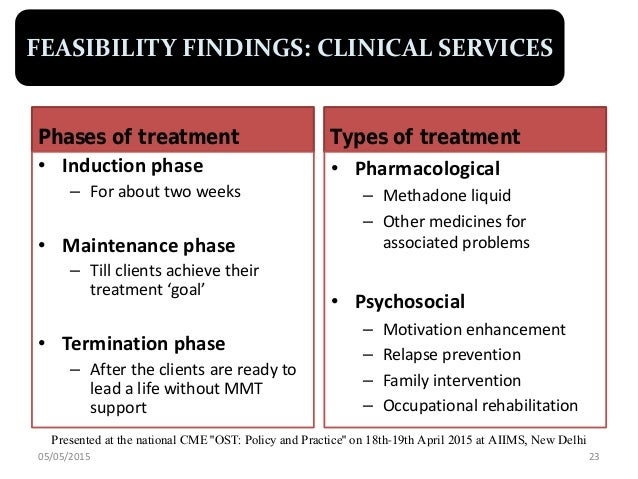
The Second Stage: Induction
Now begins the actual process of being switched from your current “street” opioid (heroin, or prescription painkillers) on to the treatment opioid medication. At the time of induction, you will be asked to provide a urine sample to confirm the presence of opioids and possibly other drugs. You should arrive to your first visit experiencing mild to moderate opioid withdrawal symptoms, that way you’ll be suitable to begin taking the treatment medication during this visit. Arrangements will be made for you to receive your first dose in a clinic or your doctor’s office, or in certain cases at home. Your response to the initial dose is usually directly monitored. In some cases you may receive additional medication, if necessary, to reduce severe withdrawal symptoms.
Since an individual’s tolerances and reactions to the treatment opioid varies, initially daily appointments may be scheduled and the medication adjusted until you no longer experience withdrawal symptoms or cravings. In the clinic setting (methadone), daily dosing appointments are usual and mandatory initially. Urine drug screening is typically required for all patients/clients initially and then randomly once each month.
Intake and Induction usually occurs at the first visit, but not always.
The Third Stage: Stabilization
Once the appropriate dose of treatment medication is established, and you are beginning to feel well throughout the 24-hour dosing interval (period following dosing), you will stay at this dose while stable blood levels of the treatment medication is attained. You and your doctor will discuss your treatment options from this point forward and you will begin to work on your individualized therapeutic treatment plan goals with counselors and therapists.
The Fourth Stage: Maintenance
Treatment adherence, compliance and progress will be monitored. Participation in some form of behavioral counseling is strongly recommended to ensure the best chance of treatment success and long-term sobriety. You are likely to have scheduled office appointments on a weekly or monthly basis. If treatment progress is good and goals are met, office/clinic visits may become less frequent. For clinic patients, by this time you may have become eligible to receive “take-home” doses to self-administer, so that you won’t be coming to the clinic on a daily basis.
The Fifth Stage: Medically supervised withdrawal (MSW) or detox from treatment med
As your treatment progresses, you and your doctor/treatment team may eventually decide that medically supervised withdrawal is now appropriate. In this phase, your doctor will gradually taper your treatment medication dose over time, taking care to see that you do not experience any withdrawal symptoms or cravings. This should be a slow and gradual process taking weeks, to months, to years for some. However long that you think that it may take you, double it, and that will probably be a more realistic time frame! The reason is that your body has become physically, physiologically dependent on the treatment opioid medication to function normally and so it has to be slowly trained to function on less and less of that opioid, which is a slow process.
Aftercare: Medical options
Medication assistance can be continued (indefinitely) after OAT has concluded. This is usually in the form of opioid antagonist therapy using Naltrexone, orally, daily, or by once-monthly injections. This medication is an opioid-blocker, not an opioid, and is not habit-forming/addictive. It blunts the effects of ingesting or using opioids and is successful in preventing relapses to a significant degree.
Another medication that should be in the possession of all recovering opioid dependent persons is Naloxone. Naloxone, like Naltrexone is an opioid-antagonist (opioid-blocker) but it has a very short duration of action and so is used only in emergency scenarios to reverse life-threatening opioid overdoses.
New, long-acting opioid-agonist Buprenorphine products (Probuphine, Subclocade) are now available which allow once monthly administration by injection (subcutaneous implantation).
After you complete MAT, if you feel that a relapse is eminent returning to some form of low-dose MAT is a preferable option to relapse. Addiction has no cure and is a chronic, relapsing, brain disorder. As such, the risk of relapse is never zero and so it is always a possibility, that is why one’s sobriety cannot be taken for granted and recovery has to become a lifestyle that is constantly being supported. Periodically having to return to MAT is not a bad thing, relapse is.
I hope you found this article informative!
